“The risk of a DVT occurring on a flight lasting more than four hours is between 1 in 4,650 flights and 1 in 6,000 flights.”
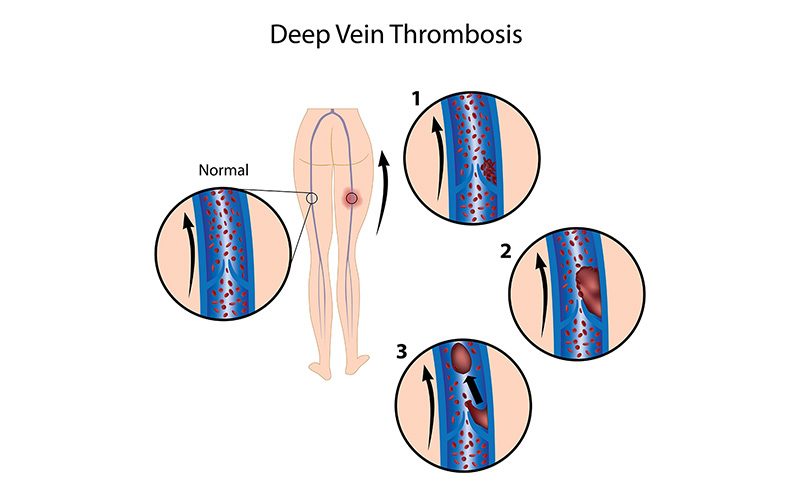
Your lungs have many functions in your body beyond just oxygenating your blood. One of their other important roles is filtering the venous blood that returns from the body. The venous system is characterized by slower blood flow than the arterial system, which contributes to the occasional formation of a blood clot (known as a “peripheral venous thrombosis”), which could be transported into the lungs and could even cause a pulmonary embolism (or blockage in the vessels of the lungs).
Dans ce chapitre, vous apprendrez ce qui suit :
Thrombose veineuse profonde

Deep vein thrombosis (DVT) is a condition in which a blood clot (a “thrombus”) forms in one or more of the body’s deep veins, usually in the legs. If a clot breaks free and travels through the circulatory system, it can lead to life-threatening conditions. For example, if a clot lodges in the lungs, it is known as a pulmonary embolism (PE) and affects the lungs’ ability to oxygenate the blood (see “Pulmonary Embolism”). Collectively, DVT and PE are sometimes referred to as venous thromboembolisms (VTEs).
A clot that originates as a DVT can also cause a stroke in individuals with a patent foramen ovale (PFO, a hole in the wall between the atria — see “Patent Foramen Ovale” for details about this condition); in such a case, the clot travels through the veins to the right atrium of the heart, passes through the PFO to the left atrium and then travels through the arteries to the brain.
La TVP n'est pas liée à la plongée, mais les plongeurs voyagent souvent et les voyages constituent un facteur de risque important pour la TVP. Dans environ la moitié des cas de TVP, l'individu ne présente aucun symptôme notable avant l'apparition de la maladie. Le plus souvent, la maladie se déclare au niveau du mollet. Les symptômes peuvent être les suivants
- Gonflement de la jambe, de la cheville ou du pied affecté
- Douleur dans le mollet qui s'étend à la cheville ou au pied
- Chaleur dans la zone affectée
- A change in the color of the skin — to pale, red or blue
La plupart des TEV liées à un voyage en avion surviennent dans les deux semaines suivant le vol et disparaissent dans les huit semaines. Si elle n'est pas traitée, une TVP qui débute dans le mollet s'étend à la cuisse et au bassin dans environ 25 % des cas. Une TVP de la cuisse et du bassin non traitée a un risque d'environ 50 % de conduire à une EP, qui est la complication la plus grave de la TVP. De nombreux cas de TVP sont asymptomatiques et se résorbent spontanément. Toutefois, la TVP réapparaît souvent chez une personne qui a déjà souffert d'un épisode de la maladie.
Most DVTs occur in individuals with pre-existing risk factors for DVT who remain motionless for a long time — such as when traveling a long distance by plane, car or train; when doing deskwork over a period of many hours; or when bedridden. This is because immobility slows down the blood flow in the veins (a condition known as “venous stasis”); in addition, pressure on the calf from an inadequate seat can injure the vein walls. If you sit still for 90 minutes, the blood flow in your calf drops by half, and that doubles your chance of developing a blood clot. For every additional hour you spend sitting, your risk of a blood clot increases by 10 percent.
The incidence of DVT in the general population is one-tenth of one percent, but it is higher in those who have risk factors and those who travel often. Long-distance air travel may double or even quadruple the risk of suffering a VTE. Although DVT is often called the “economy class disease,” business-class travelers are susceptible, too. The risk of a DVT occurring on a flight lasting more than four hours is between 1 in 4,650 flights and 1 in 6,000 flights; this is lower than the risk in the general population, but that’s because people who take long trips are likely to be healthier than average. The incidence of DVT among travelers with a low to intermediate pre-existing risk for VTE who take a journey longer than eight hours was found to be 0.3 percent for symptomatic cases and 0.5 percent when including asymptomatic cases as well.
Les facteurs de risque de la TVP sont les suivants
- L'âge avancé (le risque augmente après 40 ans)
- Obésité (définie par un indice de masse corporelle supérieur à 30)
- Utilisation d'œstrogènes (contraceptifs hormonaux ou traitement hormonal de substitution)
- Grossesse (y compris la période postnatale)
- Thrombophilie (tendance anormalement élevée du sang à coaguler)
- Antécédents de MTEV ou antécédents familiaux de MTEV
- Cancer actif
- Maladie grave
- Intervention chirurgicale, hospitalisation ou traumatisme récent
- Mobilité limitée
- Central venous catheterization (the presence of a catheter in one’s chest, for use in administering medication or nutrients and/or drawing blood samples)
Entre 75 % et 99 % des personnes qui développent une TEV liée à un voyage présentaient plus d'un de ces facteurs de risque.
Height is also a factor in one’s risk of developing a travel-related DVT. People who are either very short — less than 5 feet, 3 inches (1.6 meters) — or very tall — more than 6 feet, 3 inches (1.9 meters) — appear to be at increased risk as a result of their inability to adjust their seats sufficiently to accommodate their height. In addition to effects of immobility, shorter passengers may suffer greater than usual seat-edge pressure on the backs of their knees, and taller passengers may be cramped due to insufficient leg room. All of these factors can contribute to injury of deep veins, venous stasis and activation of the blood’s clotting mechanisms.
Those who are at increased risk of DVT should wear compression socks whenever they fly or drive long distances and should consult their primary-care provider regarding the possible benefit of taking a clot-preventative such as aspirin. Although the risk of DVT for healthy people is small, everybody should be aware of the factors that can precipitate the condition — and avoid long periods of immobility. The best way to prevent DVT is to get up and walk around from time to time. It also helps to flex your feet and calf muscles regularly if you must remain seated for any length of time. Finally, it is also helpful in preventing DVT to stay well hydrated.
Effet sur la plongée
Toute personne chez qui on a diagnostiqué une TVP aiguë ou qui prend des anticoagulants doit s'abstenir de plonger. Il est possible de reprendre la plongée en toute sécurité après une TVP, mais l'évaluation de l'aptitude à la plongée doit être faite au cas par cas.
Embolie pulmonaire
A pulmonary embolism (PE) is an obstruction (or “embolus”) that lodges in the vasculature of the pulmonary system, or lungs. The embolus may be air, fat or a blood clot (or “thrombus”). If a PE is caused by a thrombus, the clot typically originated in the deep vein system of the legs — a condition known as deep vein thrombosis (DVT); see “Deep Vein Thrombosis” for a discussion of DVT. The resulting obstruction in the flow of blood to the lungs typically causes a drop in cardiac output and a significant drop in blood pressure.

L'apparition de l'EP peut être aiguë ou chronique. L'EP aiguë provoque souvent des symptômes évidents pour l'individu, tandis que l'EP chronique ne révèle souvent sa présence que par des résultats très subtils qui sont passés inaperçus pour l'individu affecté. Une EP non traitée a un taux de mortalité élevé. Le pronostic est particulièrement sombre pour les personnes qui présentent en même temps une TVP, un thrombus du ventricule droit ou un dysfonctionnement du ventricule droit. On estime que 1,5 % des décès sont diagnostiqués comme étant dus à une EP.
Risk factors for DVT — and thus for PE — include recent surgery; a stroke; a diagnosis of autoimmune disease, malignancy or heart disease; obesity; smoking; hypertension; and a previous DVT.
Symptoms of PE include chest pain (also known as “dyspnea”), pain or swelling of the calf (signaling a DVT), hypotension (abnormally low blood pressure), an altered level of consciousness and syncope (fainting). Distension of the neck veins in the absence of other conditions — such as pneumothorax (a buildup of air in the membrane surrounding the lungs, sometimes referred to as a collapsed lung) or heart failure — may also be observed in individuals suffering a PE.
PE should be one of the first conditions considered when attempting to make a diagnosis in someone exhibiting acute onset of any of the symptoms listed above and any of the associated risk factors. Appropriate diagnostic tests may include measurement of the individual’s levels of a hormone called brain natriuretic peptide (BNP) and of a protein known as cardiac troponin, as well as a CT angiogram of the lungs.
Treatment should focus initially on managing the significant cardiopulmonary impairments that are usually involved in a PE. Such care may include breathing support from an artificial ventilator and fluid management. The use of anticoagulant medication is also important, both to treat the embolus and to stop the development of another thrombus. Thrombolysis (known as “clot-busting”), embolectomy (surgical removal of the embolus) or the placement in the vena cava (one of the large vessels in the chest) of a filter designed to prevent any future clots from reaching the lungs may also be considered — especially in anyone who goes into shock, because mortality in such cases approaches 50 percent. Similar measures may be called for in cases of PE caused by a venous gas bubble. Hyperbaric oxygen therapy may be indicated as well, if the individual’s condition does not improve or deteriorates even after the application of supportive measures.
Effet sur la plongée
Despite many medical advances, five-year all-cause mortality in individuals who have suffered a PE due to underlying risk factors remains more than 30 percent. And pulmonary hypertension — elevated pressure in the arteries that carry blood from the heart to the lungs, a condition that limits one’s exercise capacity — often persists in individuals who have had a PE, even after successful treatment. Thus any determination of fitness for diving by those who have had a PE must include an evaluation of their lung function, underlying conditions, anticoagulation status, exercise capacity and cardiac status.
Œdème pulmonaire d'immersion
Immersion pulmonary edema (IPE) is a form of pulmonary edema — an accumulation of fluid in the tissues of the lungs — that specifically affects divers and swimmers. Immersion at depth is a key factor in the development of IPE. That’s because immersion in an upright position causes a significant shift of fluid from the peripheral to the central circulatory system, resulting in higher pressure in the capillaries of the pulmonary system. Elements of the diving milieu that contribute to IPE’s occurrence include the fact that divers breathe gases that are denser than air at sea level, which means more negative pressure within chest is needed to inhale; the likelihood of gas bubbles becoming trapped in the vasculature of the lungs; the cold underwater environment; and the potential in underwater settings for exertion or panic, which can exacerbate elevated capillary pressure.

Maintaining a proper fluid balance in your lung tissue and its vasculature requires a dynamic combination of various opposing forces. Unopposed changes in any of these forces can result in a buildup of excess fluid — or edema — in your pulmonary tissue. The main variables involved in regulating this fluid balance are the following:
- Pression oncotique (forme de pression exercée par les protéines) dans les capillaires pulmonaires, les plus petits vaisseaux du système circulatoire.
- Oncotic pressure in the pulmonary system’s interstitial fluid (fluid in the cavities of your lung tissue)
- Perméabilité des capillaires pulmonaires
- Pression hydrostatique (pression d'un fluide au repos) dans les capillaires pulmonaires
- Pression hydraulique (pression d'un fluide comprimé ou pompé) dans le liquide interstitiel
- Pression dans les alvéoles, les minuscules sacs d'air des poumons.
These factors, which collectively are known as “Starling forces,” can all be quantified and placed in an equation that can then be used to calculate the net differential of
les forces.
Pulmonary edema is caused by changes in these forces — such as a drop in the levels of key proteins in the blood; leakage from the pulmonary capillaries due to sepsis (a life-threatening complication of infections); an increase in hydrostatic pressure in the pulmonary capillaries due to heart failure; and negative pressure in the alveoli due to resistance from breathing through a faulty regulator. Additional issues that can contribute to the development of pulmonary edema include side effects of some cardiovascular drugs; ARDS (acute respiratory distress syndrome, a life-threatening condition that prevents oxygen from getting to the lungs); reperfusion (a procedure that restores circulation after a heart attack or stroke); cardiomyopathy (a weakening of the heart muscle); high-altitude pulmonary edema; a pulmonary embolus (a blood clot lodged in a vessel in the lungs); re-expansion (the reinflation of a collapsed lung); pulmonary hypertension (elevated pressure in the arteries that carry blood from the heart to the lungs); lung cancer; hemorrhage (uncontrolled bleeding); and various disorders of the nervous system. Other factors can include overhydration by well-intentioned divers who have heard the conventional wisdom that dehydration is a risk factor for decompression sickness, as well as poor physical conditioning, which can result in increased negative pressure in the alveoli during deep inspiration.
Les symptômes de l'EPI comprennent des douleurs thoraciques, une dyspnée (gêne ou difficulté à respirer), une respiration sifflante et des expectorations roses et mousseuses pendant l'immersion ou peu après la sortie de l'eau. La plupart des personnes qui souffrent d'un épisode d'EPI n'avaient pas d'antécédents ou de signes significatifs indiquant une prédisposition à cette affection ; néanmoins, le risque d'EPI augmente avec l'âge, l'obésité et une pression artérielle élevée.
Once pulmonary edema occurs, hypoxia (lack of an adequate supply of oxygen) leads to constriction of the pulmonary vasculature, which worsens the cascade of ill effects. The situation can be further aggravated by the accompanying dyspnea, which, when experienced underwater, can induce panic and uncontrolled ascent to the surface — leading to overinflation of the lungs and even near-drowning.
To help differentiate immersion pulmonary edema from other conditions with similar symptoms (such as near-drowning, pulmonary decompression sickness and pulmonary overinflation syndrome), it is important to keep in mind that IPE’s onset can occur either at depth or upon reaching the surface. And it is not necessarily precipitated by aggressive diving, a rapid ascent or the aspiration of water.
Treatment for IPE should begin with removal of the affected individual from the water (to relieve the compression of the vessels in the lower extremities, allowing centrally pooled fluids to return to the extremities) and with administration of oxygen (beginning at 100 percent and later at a reduced concentration). A diuretic such as Lasix may help to reduce excess intravascular fluid, although diuresis — the body’s natural excretion of fluid — may already be under way as a result of hormonal influences. The condition usually resolves quickly in a healthy diver. Prolonged hospitalization is rarely required; if it is necessary, it’s usually due to contributing factors, such as an underlying cardiac problem.
Effet sur la plongée
Some divers have one episode of IPE and never experience the condition again, but repeated episodes are likely. Any individuals who suffer a first episode of IPE are advised to undergo a detailed examination to rule out any medical conditions that may have caused the edema and then to have a thorough discussion with their physician regarding the risks of continuing to dive. And all divers are urged to have regular maintenance on their regulators, to refrain from overhydration and to attend to proper dive planning in order to avoid exertion and panic — as well as to keep conditions such as obesity and hypertension under control.
Suivant : Chapter 7 – Issues Involving Cardiovascular Drugs >
