“While DCS is commonly thought of as a bubble disease, bubbles are probably only the gateway to a complex array of consequences and effects.”
DCS may develop when a diver’s degree of supersaturation is so high (or, stated another way, if the elimination gradient is so steep) that a controlled transfer of inert gases from the body’s tissues to the bloodstream — and then from the bloodstream to the lungs and the lungs to the environment — is not possible. If that removal process is inadequate, inert gases will come out of solution and form bubbles that can distort tissues, obstruct blood flow, cause mechanical damage (to the joints, for example) and/or trigger a cascade of biochemical responses.
Although much is known about DCS, its mechanisms of insult are still being investigated. And while DCS is commonly thought of as a bubble disease, bubbles are probably only the gateway to a complex array of consequences and effects.
In this chapter, you’ll learn about:
Signs and Symptoms of DCS
The collective insult to the body’s systems can produce symptomatic DCS. The condition’s primary effects may be evident in the tissues that are directly insulted. Its secondary effects can compromise the function of a broad range of tissues, further jeopardizing the diver’s health.
The ability to recognize the signs, or objective evidence, and the symptoms, or subjective perceptions, of DCS — and to differentiate them from signs and symptoms less likely to be associated with DCS — is important. A variety of classification systems have been established for DCS. One common approach is to describe cases as Type 1 or Type 2.
Type 1 DCS
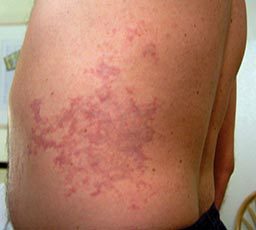
Type 1 DCS is usually characterized by musculoskeletal pain and mild cutaneous, or skin, symptoms. Common Type 1 skin manifestations include itching and mild rashes (as distinct from a clear mottled or marbled and sometimes raised discoloration of the skin — a condition that is known as cutis marmorata that may presage the development of the more serious symptoms of Type 2 DCS). Less common but still associated with Type 1 DCS is obstruction of the lymphatic system, which can result in swelling and localized pain in the tissues surrounding the lymph nodes — such as in the armpits, groin or behind the ears.

The symptoms of Type 1 DCS can build in intensity. For example, pain may originate as a mild ache in the vicinity of a joint or muscle and then increase in magnitude. However, the pain associated with DCS does not typically increase upon movement of the affected joint, although holding the limb in one position rather than another may reduce discomfort. Such pain can ultimately be quite severe.
Type 2 DCS

Type 2 symptoms are considered more serious. They typically fall into three categories: neurological, inner ear and cardiopulmonary. Neurological symptoms may include numbness; paresthesia, or an altered sensation, such as tingling; muscle weakness; an impaired gait, or difficulty walking; problems with physical coordination or bladder control; paralysis; or a change in mental status, such as confusion or lack of alertness. Inner-ear symptoms may include ringing in the ears, known as “tinnitus”; hearing loss; vertigo or dizziness; nausea; vomiting; and impaired balance. Cardiopulmonary symptoms, known commonly as “the chokes,” include a dry cough; chest pain behind the sternum, or breastbone; and breathing difficulty, also known as “dyspnea.” The respiratory complaints, which are typically due to high bubble loads in the lungs, can compromise the lungs’ ability to function — threatening the affected diver’s health, and even life, if treatment is not sought promptly.
Type 2 symptoms can develop either quickly or slowly. A slow build can actually obscure the seriousness of the situation, by allowing denial to persist. For example, fatigue and weakness are common enough concerns, especially if their onset is protracted, that they can be very easy to ignore. Less common symptoms, such as difficulty walking, urinating, hearing or seeing — especially if their onset is quick — can sometimes prompt faster recognition of the existence of a problem. It is fair to say that divers can initially be reluctant to report symptoms, though they usually will do so if their symptoms do not go away. This is a shortcoming divers should be aware of, lest they fall prey to it.
Presentation of DCS
The presentation of DCS is frequently idiosyncratic — that is, its “typical” pattern can be atypicality. In some cases, an affected diver’s chief complaint may draw attention away from more subtle but potentially more important symptoms. The following list ranks the initial manifestations of DCS, from those most commonly to least commonly reported (Vann et al. 2011):
- Pain, particularly near the joints
- Numbness or paresthesia
- Constitutional concerns — such as headache, lightheadedness, unexplained fatigue, malaise, nausea and/or vomiting, or anorexia
- Dizziness or vertigo
- Motor weakness
- Cutaneous, or skin, problems — such as an itch, rash, or mottling (“cutis marmorata”)
- Muscle discomfort
- Impaired mental status
- Pulmonary problems — such as breathing difficulties (“the chokes”)
- Impaired coordination
- Reduced level of consciousness
- Auditory symptoms — such as hearing sounds that are not there or having a hard time hearing
- Lymphatic concerns — such as regional swelling
- Bladder or bowel dysfunction — such as retention of urine
- Compromised cardiovascular function
According to this recent review, pain and numbness, also known as paresthesia, were reported initially in nearly two-thirds of cases of DCS, constitutional symptoms in approximately 40 percent of cases, dizziness/vertigo and motor weakness in approximately 20 percent, and cutaneous symptoms in approximately 10 percent (Vann et al. 2011).
Differential Diagnosis of DCS

DCS is a high-profile diving injury because of its potential severity. But divers need to remember that not all diving-related problems turn out to be DCS. When two or more conditions have overlapping symptoms, as is the case with many diving-related injuries, differential diagnosis is the process by which medical personnel figure out which of the potential conditions is most likely responsible for the symptoms.
The term decompression illness (DCI) was coined to encompass both DCS and the related condition known as arterial gas embolism (AGE), the latter arising from barotrauma of the lungs that introduces gas into the systemic bloodstream. Some of the other conditions and circumstances that involve similar symptoms include inner-ear barotrauma; middle-ear or maxillary sinus overinflation; contaminated breathing gas; oxygen toxicity; musculoskeletal strains or trauma sustained before, during or after a dive; marine life envenomation; immersion pulmonary edema; water aspiration; and coincidental neurological disorders, such as stroke (Vann et al. 2011). Thermal stress — sometimes due to excessive heat, but usually due to cold exposure — can also be responsible for similar symptoms. In some cases, a careful medical history can easily rule out one diagnosis or another. For example, symptoms of immersion pulmonary edema often develop at depth. In such a case, a good history would rule out DCS, which only develops after significant decompression stress during ascent.
It is essential for divers with any of these symptoms to seek medical evaluation and support. While first responders are able to perform initial analysis of an injured individual, such as administering a field neurological assessment, the capabilities of nonphysicians do not come close to the clinical skills and insights held by experienced clinical specialists.
