DAN MEDICS AND RESEARCHERS ANSWER YOUR DIVE MEDICINE QUESTIONS.
Q: When can I return to diving after carpal tunnel surgery?
A: You need to be completely healed following surgery, which will require time, depending on the severity of the carpal tunnel syndrome and the surgical procedure utilized. Everyone heals differently. Your surgeon will monitor the healing process through follow-up appointments and can estimate your progress.
You may also need physical therapy to return your hand to full function. Diving is equipment-intensive, and any strength, dexterity, or fine motor control deficits could cause a safety concern for you and your dive group. You must be able to operate all your equipment — such as gauges, buckles, weights, and valves — without restrictions or limitations.
Wearing a drysuit or wetsuit will compress the area around your wrist. This compression can irritate any surgical site that is not completely healed.
An operation involving nerves and tendons does not generally impose any restrictions on diving once you are fully healed and released by your physician for unrestricted activity. Ideally, you should have no motor or sensory deficit, even during rigorous activity or normal wristband or wetsuit wear. Mild and stable sensory deficits may occasionally persist and require a physician’s clearance before diving.
After any surgery there is a theoretical concern of an increased risk of bubble formation where there has been some disruption of blood supply that leaves increased or decreased vascularity. There have been no studies to prove or disprove this theory.
If you are cleared to dive, we recommend noting any neurological deficits and disclosing them to your dive buddy, dive operator, and anyone else who may need to decide on proper assessment and treatment recommendations following a dive injury. Confusing a symptom with a preexisting condition when it is a symptom of a new condition could delay or lead to incorrect treatments.
— Jevon Monaghan, EMT-P
Q: After doing three dives with a somewhat dry throat, I developed uvulitis. It was quite severe, making it difficult to swallow. Is there research on this condition in diving? My main concern is that swelling may impair an airway.
A: There is no specific research on uvulitis in diving. A handful of anecdotal cases exist online of divers who experienced a sore throat or swelling of the uvula after repetitive diving. Any condition that affects the airway warrants prompt medical attention.
Causes for airway issues range from benign to serious, including allergies, dehydration, medications, infections, and genetic factors. While diving should not be the sole cause, it can facilitate some of the causes associated with uvulitis, such as potential exposure to allergens or infectious agents. Continuously breathing dry gases can worsen the situation.
In addition to breathing concerns, you may have difficulty with equalization. Consulting an ear, nose, and throat physician may be warranted if the condition recurs, and it’s imperative for any condition with concern about your airway.
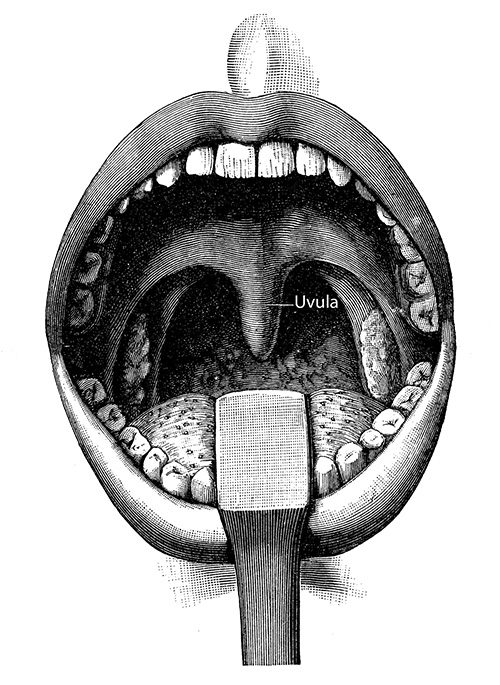
If you notice a sore throat after diving, refrain from diving until you are evaluated and treated and your symptoms have resolved to prevent exacerbating the condition or transmitting it to others if infectious.
— Shannon Sunset, NCPT, AEMT
Q : I recently had a UroLift procedure. Can I return to diving?
A: An enlarged prostate, or benign prostatic hyperplasia (BPH), is more common as men age, affecting approximately 500 million men worldwide. This condition can cause bothersome urinary symptoms. The UroLift is a minimally invasive procedure to get enlarged tissue out of the way and alleviate BPH symptoms. Lifting and pinning back enlarged prostate tissue stops it from blocking the urethra and obstructing urine flow.
UroLift implants are made of solid materials and will not likely be problematic while diving, barring complications. Antidepressants, antihistamines, bronchodilators, anticholinergics, and sympathomimetics, however, may worsen BPH symptoms. These medications can tighten prostate and bladder neck muscles, causing difficulty with urination, which can pose a diagnostic challenge because the inability to urinate can be a symptom of serious decompression sickness (DCS).
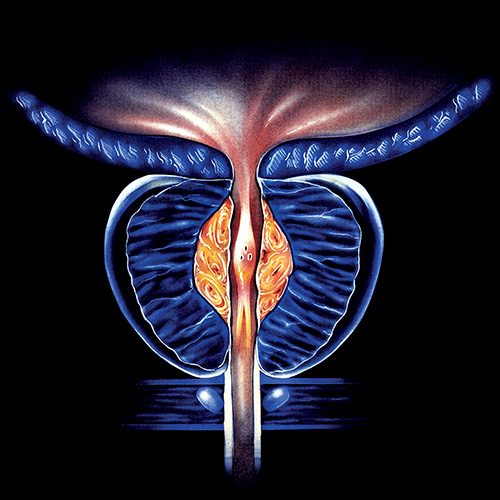
Any additional medication following this procedure may bring additional considerations. The recommendation with any procedure is to be cleared by your treating physician for full and unrestricted activity before returning to diving after healing.
— Leandra Lynn, NREMT