Proceedings Summary | DAN and UHMS Medical Examination of Diving Fatalities Symposium
Introduction
The DAN/ Undersea & Hyperbaric Medical Society (UHMS) sponsored Medical Examination of Diving Fatalities Symposium was held on June 18, 2014 in St. Louis, Missouri. Although the symposium was geared towards medical examiners, many of the issues discussed in the workshop are pertinent to dive professionals.
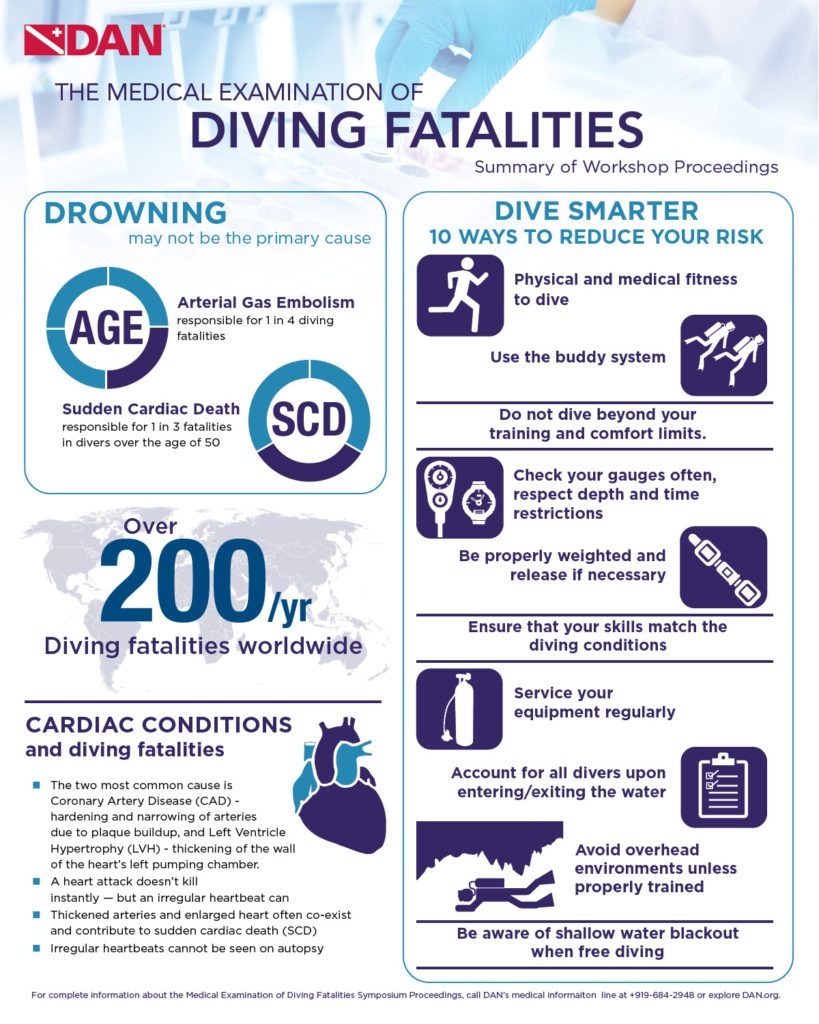
Why It May Not Be Drowning
- A large number of deaths in scuba ascribed to drowning are in fact due to other causes: specifically, sudden cardiac death (SCD), and to a lesser extent, arterial gas embolism (AGE).
- Some cases which have been labeled as “immersion” or “drowning” have subsequently been found to be due to other causes. Some of the more unusual causes include inhalation of inert gas (nitrogen), air hose entanglement (entrapment), and cuttlefish attack that caused perforated tympanic membrane, leading to panic, rapid ascent and gas embolism; there were also other causes labeled drowning.
- Most medical examiners would call it drowning, simply because someone was in the water.
Cardiac Conditions Are Common Causes
- Sudden cardiac death (SCD): two most common causes of SCD sudden causes in adults are coronary artery disease and left ventricle hypertrophy (LVH).
- Atherosclerotic heart disease: it is not the heart attack that kills the person instantly, heart attacks and subsequent damage to the myocardium kill people over a time course of hours to days. It is the dysrhythmia that kills people instantly.
- You can’t see an arrhythmia on autopsy.
- Left Left ventricular hypertrophy (LVH): atherosclerotic disease often co-exists with another risk factor for SCD and that LVH. If you don’t recognize it, you are missing a huge risk factor for sudden death.
- LVH may play a significant role in SCD in divers due to the stress on the body from diving may precipitate arrhythmias and death.
- If we know what risk factors to look for, we may be able to improve our fitness to dive screenings and potentially prevent some of these deaths.
Looking for Preventable Causes of Death
- Fatality investigation: in most cases investigation usually ends with establishing proximal cause of death. Unintentional or natural cause of death investigation usually stops short of pursuing root causes.
- Injury research depends on the quality of data pro vided by investigation. Legal investigation may provide answers on questions of how it happened but often not concerned with “why”. The medical examination may answer what were the cause of death and the mode of death.
Field Investigations: Preserving the Evidence
Three general patterns to a diver’s death:
- First, death occurs underwater with no rescue or resuscitation attempted. Disadvantage by possible delay in between when the diver dies and is recovered – autopsy info can be altered or affected.
- Second, diver has a triggered even in the water and is brought to shore or boat for attempted rescue but dies prior to transportation to medical facility. Usually provides a witness to describe what happened.
- Third, diver is transported to a medical facility and survives for a few hours or days. Advantages are that imaging and lab tests may guide determination of the cause of death, however autopsy findings may be altered by the survival interval and medical intervention.
Diving conditions and diving equipment may cause or contribute to a diver’s death. Information may be lost as witnesses leave, forget equipment, or worse, equipment is returned to the family.
Field investigation is categorized into six parts:
- History
- Antemortem events
- The environment
- Body recovery
- Medical care administered before death
- Body and equipment recovery and documentation and preservation of evidence
Post Mortem: How-To
- Very few forensic pathologists have significant experience with the investigation of fatalities involving divers who were breathing compressed gas.
- Fewer than 100 combined deaths occurring in the US, Canada, and the Caribbean each year.
- Pathologists should be aware of the circumstances surrounding the fatal dive mishap, but the diver’s past medical and surgical history, recent health status, and any medications taken on a regular basis and on the day of the mishap need to be known.
- Cardiovascular disease in particular is a frequent factor in a diving related fatality, especially in older divers.
What Medical Examiners Need to Know About Rebreathers
- Three main root causes of fatal accidents with rebreathers:
- Diver error (the most common)
- Mechanical problems
- Electronic problems
- An autopsy cannot reveal hypoxia, hyperoxia, or hypercapnia (the three most common causes of rebreather fatalities). In most cases, the medical examiner cannot detect the root cause of a rebreather fatality.
Expert Panel Review of Investigation and Autopsy Findings
Guidelines identified by common trends seen in diver death:
- Ensure physical fitness to dive: train for your sport and be sure that you exercise regularly and follow a healthy diet.
- Use the buddy system.
- Follow your training: check your gauges often, respect depth and time restrictions, and do not dive beyond your training limits.
- Weight yourself properly and remember to release your weights when appropriate.
- Ensure that your skill level and familiarity are appropriate for conditions.
- Have your equipment serviced and maintained regularly.
- Account for all divers (a physical, individual response should be received from every diver before entering/after exiting).
- Avoid overhead environments unless properly trained and equipped.
- Breath-hold divers should remember to use the buddy system and be aware of the dangers of shallow-water blackout.
Denoble PJ (editor). Medical Examination of Diving Fatalities Symposium Proceedings. Durham, NC, Divers Alert Network, 2015, 64 pp.

Appendix F in the Recreational Diving Fatalities Workshop Proceedings is the Autopsy Protocol for Recreational Diving Fatalities by Dr. James Caruso
Vann RD, Lang MA, eds. Recreational Diving Fatalities. Proceedings of the Divers Alert Network 2010 April 8-10 Workshop. Durham, NC: Divers Alert Network, 2011. IBSN#978-0615-54812-8.
History
This is absolutely the most important part of the evaluation of a recreational diving fatality. Ideally, one should obtain significant past medical history with a special focus on cardiovascular disease, seizure disorder, diabetes, asthma and chronic obstructive pulmonary disease. Medications taken on a regular basis as well as on the day of the dive should be recorded, and information regarding how the diver felt prior to the dive should be obtained. Any history of drug or alcohol use must also be noted.
The dive history is extremely important. If possible, the investigator should find out the diver’s experience and certification level. The most important part of the history will be the specific events related to the dive itself. The dive profile (depth, bottom time) is an essential piece of information, and if the diver was not diving alone, eyewitness accounts will be invaluable. With the near-universal use of dive computers, the computer used by the deceased diver should be interrogated, and if it has a download function all recent dives should be reviewed.
Not only will the last dive or dive series be invaluable to the investigation, much can be learned about the diver by looking at previous dives made, including frequency, depth, ascent habits and with certain computers even breathing gas usage. Written dive logs are also a valuable source of information related to the diver’s experience level and dive habits.
Questions Include:
- When did the diver begin to have a problem (predive, descent, bottom, ascent, postdive)?
- Did the diver ascend rapidly (a factor in air embolism and pulmonary barotrauma)?
- Was there a history of entrapment, entanglement or trauma?
- If resuscitation was attempted, what was done, and how did the diver respond?
External Examination and Preparation
A thorough external examination including documentation of signs of trauma or animal bites or envenomation should be carried out. Palpate the area between the clavicles and the angles of the jaw for evidence of subcutaneous emphysema. X-rays of the head, neck, thorax and abdomen should be taken to look for free air. Postmortem CT imaging can be obtained as an alternative.
Modify the initial incision over the chest to make a “tent” or “pocket” out of the soft tissue (an “I” shaped incision) and fill this area with water. A large bore needle can be inserted into the second intercostal spaces on each side; if desired, any escaping air can be captured in an inverted, water-filled, graduated cylinder for measurement and analysis. As the breast-plate is removed, note any gas escaping from vessels. An alternative test for pneumothorax consists of teasing through the intercostal muscles with a scalpel and observing the relationship between the visceral and parietal pleura as each pleural cavity is entered. If the two pleural layers are still adjacent until the pleural cavity is breached, there is no evidence of a pneumothorax. If a pneumothorax had occurred during the final dive, the lung would already be at least partially deflated and not up against the parietal pleura.
The pericardial sac can be filled with water and the chambers of the heart may be incised with a scalpel to look for any intracardiac gas. As was possible for the pleural cavities, escaping gas may be captured and analyzed, but most medical examiner offices do not have the resources for such endeavors. After the mediastinum, heart and great vessels have been examined under water for the presence of gas, the water may be evacuated and a standard autopsy may be performed.
Carefully examine the lungs for bullae, emphysematous blebs and hemorrhage.
Note any interatrial or interventricular septal defects. Carefully check for evidence of cardiovascular disease and any changes that would compromise cardiac function.
Toxicology: Obtain blood, urine, vitreous, bile, liver and stomach contents. Not all specimens need to be run, but at least look for drugs or abuse. If an electrolyte abnormality is suspected or if the decedent is a diabetic, the vitreous fluid may prove useful for analysis.
Prior to opening the skull, tie off all the vessels in the neck to prevent artifactual air from entering the intracranial vessels. Tie the vessels at the base of the brain once the skull is opened. Disregard bubbles in the superficial veins or venous sinuses. Examine the meningeal vessels and the superficial cortical vessels for the presence of gas. Carefully examine the Circle of Willis and middle cerebral arteries for bubbles.
Have an expert evaluate the dive gear. Are the cylinders empty? If not, the gas should be analyzed for purity (a little carbon monoxide goes a long way at depth). All gear should be in good working order with accurate functioning gauges.
Possible Findings
Air Embolism
Intra-arterial and intra-arteriolar air bubbles in the brain
and meningeal vessels, petechial hemorrhages in gray and
white matter, evidence of COPD or pulmonary barotrauma (pneumothorax, pneumomediastinum, subcutaneous emphysema), signs of acute right heart failure, pneumopericardium, air in coronary and retinal
arteries.
Carbon Monoxide Poisoning
Deaths due to carbon monoxide poisoning are rare in recreational diving, but they do occur. Autopsy findings are similar to carbon-monoxide-related deaths in other settings, with the classic finding of a cherry red color to the organs and blood. A carboxy-hemoglobin measurement should be obtained as routine toxicology in all diving- related deaths to exclude the contribution of contaminated breathing gas.
Decompression Sickness
Lesions in the white matter in the middle third of the spinal cord including stasis infarction, if there is a patent foramen ovale (or other potential right to left heart shunt) a paradoxical air embolism can occur due to significant venous bubbles entering the arterial circulation.
Drowning
While drowning essentially remains a diagnosis of exclusion, there are some anatomic findings that are observed with considerable frequency. The lungs usually appear hyperinflated and can even meet at the midline when the anterior chest wall is removed. Lungs are typically heavy and edematous, and pleural effusions may be present. A moderate amount of water and even some plant material may be present, not only in the airway but also in the esophagus and stomach. Dilatation of the right ventricle of the heart is commonly observed as is engorgement of the large central veins. Fluid is also often found in the sphenoid sinus.
Venomous Stings or Bites
A bite or sting on any part of the body, unexplained edema on any part of the body, evidence of anaphylaxis or other severe allergic reaction.
Interpretation
The presence of gas in any organ or vessel observed at the autopsy of someone who breathed compressed gas just prior to death is not conclusive evidence of decompression sickness or air embolism. During a dive, especially one of considerable depth or bottom time, inert gas dissolves in the tissues, and the gas will come out of solution when the body returns to atmospheric pressure. This, combined with postmortem gas production, will produce bubbles in tissue and vessels. The phenomenon has caused many experienced pathologists to erroneously conclude that a death occurred due to decompression sickness or air embolism.
Intravascular bubbles present predominantly in arteries and observed during an autopsy performed soon after the death occurred is suspicious for air embolism. The dive history will help support or refute this theory.
Gas present only in the left ventricle or if analysis shows the gas in the left ventricle has a higher oxygen content than that present on the right side would also be supportive for the occurrence of an air embolism.
Intravascular gas from decomposition or off-gassing from the dive would contain little oxygen and be made up of mostly nitrogen and carbon dioxide.
Deeper, longer dives can cause decompression sickness and significant intravascular (mostly venous) gas. Decompression sickness is rarely fatal and more commonly causes significant morbidity (illness and injury) in severe cases. Rapid ascents and pulmonary barotrauma are associated with air embolism.
Diving Fatalities Infographic